Organs-on-a-chip (OOC) is a 3-D microfluidic cell culture chip which mimics or replicates the physiological response of actual organs or organ systems of the human body. Some organs that have been successfully simulated by microfluidic devices are kidney, artery, bone, cartilage, skin, lung, and heart amongst others.
A typical challenge faced by the use of such devices is in measuring the electrical functions of cells grown within these devices that are electrically active like the neuronal cells in the brain or beating heart cells. This creates trouble in determining the electrical activities and the differentiation status of these cells. A team at the Wyss Institute for Biologically Inspired Engineering led by Don Ingber collaborated with Wyss Core Faculty member Kit Parker and his group in addressing these problems.
The plan was to fit these chips with embedded electrodes using new layer-by-layer fabrication process that allow exact and constant monitoring of what is known as the transepithelial electrical resistance (TEER). The TEER is the measurement of electrical resistance across a cellular monolayer and is a highly sensitive and genuine way of assuring the integrity and permeability of the monolayer.
In this novel electrically active Organ Chips, the TEER measurement will quantify the flow of ions between the electrodes and across the tissue-tissue interface made of an organ-specific epithelium (epithelial cells which construct the tissues) and endothelium (epithelial cells which line the blood vessels). The advancements don’t stop here. The team went a step forward by enhancing the functionality of the TEER chips by merging Multi-Electrode-Arrays (MEAs) in the chips that can now easily assess the behaviour of electrically active cells like beating heart muscle cells. This system was tested by developing a vascularized Heart Chip in which human cardiomyocytes are cultured in one microfluidic channel that is separated by a thin semi-permeable membrane from a second, parallel endothelium-lined vascular channel. And the working of this chip was tested using a known inflammatory agent that specifically disrupts endothelial barriers and act directly on cardiomyocytes.
Cardiomycetes (microscopic image)
(Source:humpath.com)
“This new chip enables us to perform live electrophysiological measurements to assess the integrity of the endothelial barrier in the heart using TEER measurements, while simultaneously quantifying the beating frequency of the heart cells using MEA. This allows us to reveal how drugs affect heart functions in a scenario where the two cell populations are closely coupled,” said a team member (source: wyss.harvard.edu)
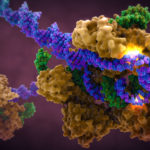
TEER-MEA chip (the TEER electrodes in gold)
(Source: wyss.harvard.edu)
Whether it is with regards to this chip in particular or other such equivalents, in general, there are couples of disadvantages, like when it comes to drug testing some properties of the drug like encapsulation and release, and signal-to-noise ratio may not be measured or categorized with such devices. The system may be both difficult and costly to construct. And is very less likely to be reusable. Some key advantages, however, are its fantastic ability and potential to replace animal testing successfully. They may also become cheaper and easier to handle in the long run shall such research continue to attract engineers and funding sources.
Reference:
wyss.harvard.edu/wyss-institutes-organ-chips-get-smart-and-go-electric/