The COVID-19 pandemic caused by the serious acute respiratory syndrome coronavirus 2 (SARS-CoV-2), is of a scale unheard of since the 1918 flu pandemic. Even though its overwhelming clinical introduction is with a respiratory infection, neurological signs are being perceived increasingly. Based on information of different coronaviruses, particularly those that caused the severe acute respiratory syndrome and Middle East respiratory syndrome epidemics, instances of the central nervous system and peripheral nervous system illness brought about by SARS-CoV-2 may be thought to be uncommon. However, the respiratory symptoms are just one side of the coin.
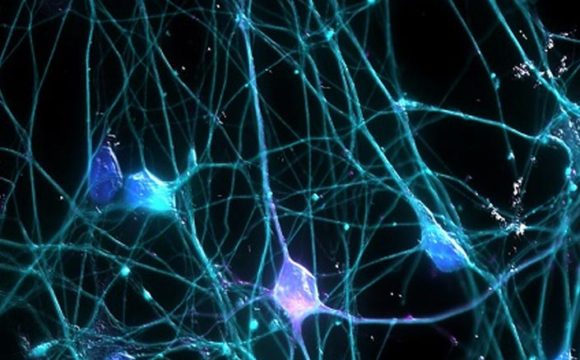
The coronavirus SARS-CoV-2 gets attached to some molecules like a key on the surface of the host cell opening doorways to the insides of cells. The entry of the virus into the host cells creates an enormous immune response. Quite a bit of this fight is pursued inside the lungs, which clarifies why numerous patients hospitalized with COVID-19 have extreme respiratory side effects. But recently expanding proof suggests blood vessel inflammation as crucially affecting the severity of COVID-19. Moreover, somewhere in the range of 30 to 80 percent of patients experience neurological indications as well as symptoms. The neurological symptoms include dizziness, headache, nausea, and loss of concentration and these symptoms tell that SARS-CoV-2 also affects cells of the central nervous system. While there is no proof yet that the infection attacks the brain, the researchers at the Lewis Katz School of Medicine at Temple University suggests that the spike proteins extruding from SARS-CoV-2 induce inflammatory responses on the endothelial cells that comprise the blood-brain barrier. Their publication is the first to show that SARS-CoV-2 spike proteins can make this barrier “leaky,” conceivably disturbing the fragile network of neurons inside the brain.
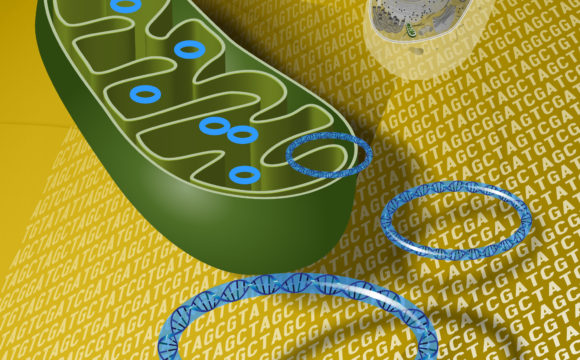
Usually, the SARS-CoV-2 utilizes its spike proteins to infect the host cells. These proteins bind to the ACE2 i.e. Angiotensin Converting Enzyme which is present on the surface of the host cell. ACE2 is known to be expressed on the endothelial cells, which structure the inward lining of blood vessels, and has a significant role in carrying out various functions of the cardiovascular framework. Since ACE2 is a crucial binding target for SARS-CoV-2 in the lungs as well as the vasculature of different organs, tissues present behind the vasculature that gets blood flow from affected vessels, can be damaged from the virus. It is yet to be unfolded whether the ACE2 also exists in the cerebrum vasculature or whether its expression results in worsened COVID 19 conditions and increased health issues like high blood pressure (hypertension). To find this a team of scientists examined postmortem human brain tissue for the expression of vascular ACE2 utilizing tissues from people without basic medical issues and from people in whom hypertension and dementia had been found and it indicated that ACE2 is expressed all through the blood vessels in the brain’s frontal cortex and is fundamentally expanded in the cerebrum vasculature of individuals with a background marked by hypertension or dementia.
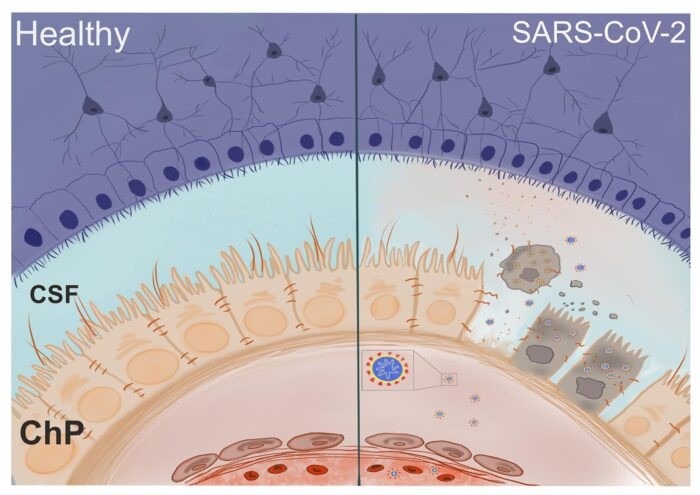
Some researchers also went into investigating the effects of the SARS-CoV-2 spike proteins on the endothelial cells of the brain in cell culture models. The establishment of the spike protein, especially in a portion known as subunit 1, created generous changes in the function of the endothelial barrier that prompted a decrease in the integrity of the barrier. The researchers additionally revealed proofs that subunit 2 of the SARS-CoV-2 spike protein can straightforwardly affect the function of the blood-brain barrier and this is of significance in light of the fact that unlike subunit 1, subunit 2 of the spike protein doesn’t tie to ACE2, implying that penetration to the blood-brain barrier could take place in a way that is independent of ACE2.
Servio H. Ramirez, Ph.D., Professor of Pathology and Laboratory Medicine at the Lewis Katz School of Medicine at Temple University and principal investigator of this study concluded that the spike proteins of the SARS-CoV-2 present and circulating in the circulatory system, could destabilize the blood-brain barrier in major areas of the brain and its modified functions of the barrier, which typically keeps harmful agents out of the cerebrum, incredibly builds the chance of neuro-intrusion by this virus, offering a clarification for the neurological signs experienced by COVID-19 patients. However, the long-term impacts of the modified function of the blood-brain barrier are yet to be discovered. It also stays obscure whether the infection can really invade neurons or glial cells that lie past the barrier. The brain vasculature is incredibly branched, so even a limited quantity of neuroinflammation can be extremely damaging and this damage could be broad in COVID-19 patients with previously existing health issues in which the vasculature has just suffered some amount of injury.
Generally speaking, the extent of patients with neurological symptoms is less in comparison to respiratory illness. Nonetheless, the proceeding pandemic, and the estimation that 50–80% of the total populace may be contaminated before the development of herd immunity, propose that the general number of patients with neurological sickness could turn out to be enormous. Neurological complications, especially encephalitis and stroke, can result in lifelong disability, with related long-term care needs and conceivably greater health, social, and monetary expenses. Medical services organizers and policymakers should know about the developing burden. Cautious clinical, epidemiological, and diagnostic investigations are expected to help characterize the neurological disease manifestations and burden.
REFERENCES:
- https://www.labroots.com/trending/microbiology/19085/sars-cov-2-disrupts-blood-brain-barrier
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7146689/
- https://www.drugtargetreview.com/news/75211/sars-cov-2-can-disrupt-the-blood-brain-barrier-find-scientists/
- https://www.thelancet.com/journals/laneur/article/PIIS1474-4422(20)30221-0/fulltext
- https://www.neurologyindia.com/article.asp?issn=0028-3886;year=2020;volume=68;issue=3;spage=560;epage=572;aulast=Garg